Polycystic Ovary Syndrome (PCOS) is a multifaceted condition that can impact various aspects of a woman’s health. This article gets to the intricacies of PCOS, offering valuable insights and shedding light on its causes, symptoms, diagnosis, and treatment options. The aim is to present complex information in an accessible and engaging manner, catering to a diverse readership.
An Overview
Polycystic Ovary Syndrome is a complex endocrine condition that affects numerous women worldwide, impacting their appearance, menstrual cycle, fertility, and hormone levels. This section provides a comprehensive overview of what PCOS is and how it manifests in affected individuals.
Polycystic Ovary Syndrome is a prevalent endocrine disorder that predominantly affects women of reproductive age. It is characterized by a myriad of symptoms, ranging from hormonal imbalances to irregular menstrual cycles, which can significantly impact a woman’s quality of life.
The complexity of PCOS lies in its multifactorial nature, involving both genetic and environmental factors. While the exact cause remains elusive, the condition is known to affect various bodily systems, including the reproductive and metabolic systems, leading to long-term health implications if left unaddressed.
Prevalence and Impact
Studies indicate that PCOS is a common condition, affecting approximately 10% of women worldwide. However, the prevalence may be higher due to underdiagnosis and misdiagnosis, highlighting the need for increased awareness and understanding of this condition.
The impact of PCOS is profound, affecting both physical and emotional well-being. Women with PCOS often experience difficulties in conceiving, along with a host of other symptoms such as weight gain and mood swings, which can lead to decreased self-esteem and mental health issues.
Causes of PCOS
The causes are multifaceted and largely unknown, with evidence suggesting a combination of genetic and environmental factors. This section explores the potential causes and risk factors associated with the development of PCOS, providing insights into its complex etiology.
Genetic Links and Risk Factors
The cause of PCOS is largely unknown, but there is substantial evidence pointing towards a genetic link. Individuals with a family history are at an increased risk, suggesting that the condition may be hereditary.
- Genetic Predisposition: A family history of PCOS or related conditions can significantly increase the risk of developing PCOS.
- Environmental Factors: Lifestyle and environmental factors such as diet and exposure to certain chemicals may also play a role in the development.
- Insulin Resistance: Many women with have insulin resistance, which can contribute to elevated levels of insulin and androgens, exacerbating the symptoms of PCOS.
Hormonal Imbalances
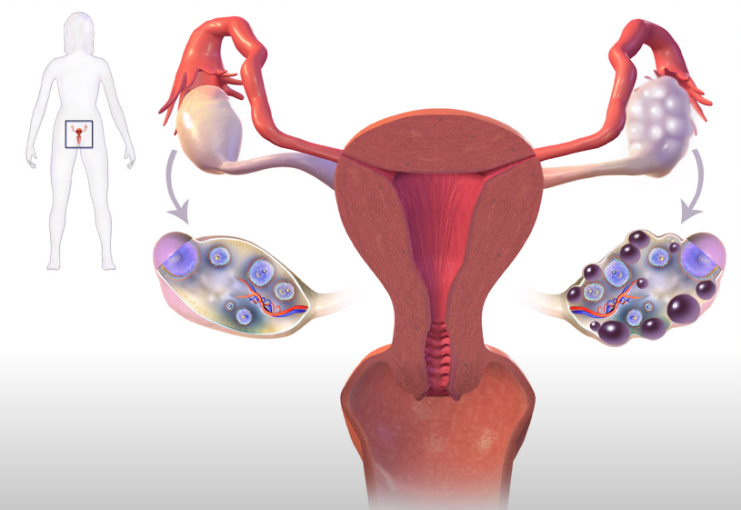
At the core of PCOS are hormonal imbalances, particularly elevated levels of androgens, also known as male hormones. These imbalances can disrupt the normal menstrual cycle and lead to the development of ovarian cysts.
- Elevated Androgens: High levels of androgens can lead to symptoms such as excessive hair growth, acne, and irregular periods.
- Insulin Imbalances: Elevated insulin levels can increase the production of androgens and contribute to insulin resistance, a precursor to type 2 diabetes.
Identifying: Symptoms and Diagnosis

Diagnosing PCOS can be challenging due to the diversity of symptoms that may vary from individual to individual. This section outlines the common symptoms associated with PCOS and the diagnostic criteria used by healthcare professionals to identify this condition.
Recognizing the Symptoms
The symptoms of PCOS are diverse and can range from mild to severe. They are primarily linked to abnormal hormone levels and can manifest in various ways, affecting menstrual cycles, physical appearance, and mental health.
- Menstrual Irregularities: Infrequent, absent, or irregular menstrual periods are common in women with PCOS.
- Fertility Issues: PCOS is a leading cause of female subfertility, often due to the lack of ovulation.
- Physical Symptoms: Excessive hair growth, acne, and weight gain are also prevalent symptoms.
- Emotional Impact: The condition can lead to depression and mood swings, impacting the overall quality of life.
Diagnostic Criteria and Challenges
Diagnosing PCOS is often a complex process, involving a thorough evaluation of symptoms, medical history, and clinical tests. The varied presentation of symptoms can make diagnosis challenging, emphasizing the importance of a comprehensive approach to identification and management.
- Clinical Evaluation: A detailed assessment of medical history, physical examination, and blood tests are crucial for diagnosing PCOS.
- Ultrasound Scan: An ultrasound may be conducted to assess the ovaries and detect the presence of cysts.
- Exclusion of Other Conditions: Other causes of menstrual disturbances and hyperandrogenism, such as thyroid dysfunction, must be excluded before confirming a diagnosis.
Navigating Fertility Challenges
Subfertility is a common concern for many women with PCOS. This section will explore how affects fertility, the underlying reasons for subfertility in women with this condition, and the interventions available to address these challenges.
Subfertility
Subfertility is often associated with PCOS, primarily due to irregular ovulation. The condition is the most common cause of female subfertility, making it a significant concern for women wishing to conceive.
Understanding the link between and subfertility is crucial for effective management. The lack of ovulation is usually the primary reason for subfertility in women with PCOS, necessitating medical interventions and lifestyle modifications to improve fertility outcomes.
Interventions and Preconception Counseling
Before any intervention is initiated for women with, preconception counseling should be provided, emphasizing the importance of lifestyle modifications such as weight reduction, exercise, reduction in smoking, and alcohol consumption.
- Ovulation Induction: Clomiphene is the recommended 1st line treatment for inducing ovulation, with patients being informed about the increased risk of multiple pregnancies.
- Advanced Interventions: For those resistant to clomiphene, exogenous gonadotrophins or laparoscopic ovarian surgery may be considered as 2nd line interventions, with in vitro fertilization (IVF) being a 3rd line intervention.
Managing Symptoms and Improving Quality of Life
Managing the symptoms is pivotal in improving the quality of life for affected individuals. This section delves into the various treatment options available, focusing on both pharmacological interventions and lifestyle modifications.
Pharmacological Interventions

Pharmacological interventions are often employed to manage the symptoms and address the underlying hormonal imbalances. These interventions are tailored to individual needs, considering the severity and range of symptoms.
- Metformin: While not recommended as monotherapy for ovulation induction, metformin can be beneficial, especially for women with insulin resistance.
- Hormonal Contraceptives: These can help regulate menstrual cycles and manage symptoms such as acne and excessive hair growth.
Lifestyle Modifications and Support
Lifestyle modifications are integral in managing PCOS symptoms and preventing long-term health complications. Supportive measures, including counseling and support groups, can also play a vital role in addressing the emotional impact.
- Healthy Lifestyle: A balanced diet, regular exercise, and weight management are crucial in managing and reducing the risk of associated health conditions.
- Mental Health Support: Addressing the psychological impact of PCOS is essential, with counseling and support groups providing valuable resources for emotional well-being.
Long-Term Health Implications
PCOS is associated with several long-term health issues, including insulin resistance, diabetes, and cardiovascular diseases. This section will explore these implications and provide insights into preventive measures and regular health checks essential for women with PCOS.
PCOS and Metabolic Complications
Women with PCOS are at an increased risk of developing metabolic complications such as insulin resistance and diabetes. Regular monitoring and management of these conditions are crucial to prevent severe health outcomes.
- Insulin Resistance and Diabetes: 10-20% of women with PCOS go on to develop diabetes, necessitating regular glucose tolerance tests and management of insulin levels.
- Cardiovascular Risks: The elevated risk of high blood pressure and heart disease in women with PCOS is often linked to other health conditions like diabetes and hypertension.
Preventive Measures and Regular Check-ups
Regular health checks and preventive measures are paramount in managing the long-term health risks associated with PCOS. These include assessing cardiovascular risk factors and adopting a healthy lifestyle to mitigate these risks.
- Regular Monitoring: Women with should undergo regular check-ups to monitor blood pressure, cholesterol, triglycerides, and HDL cholesterol levels.
- Healthy Lifestyle and Diet: Adopting a healthy lifestyle, including a balanced diet and regular exercise, is essential in preventing long-term health complications associated with it.
FAQ
Can it be cured?
Currently, there is no cure for PCOS. However, symptoms can be managed effectively with lifestyle modifications, medications, and other interventions, allowing individuals to lead a normal and healthy life.
Can it occur in postmenopausal women?
While PCOS is a condition primarily affecting women of reproductive age, the metabolic and cardiovascular risks associated with it can continue to affect women in postmenopause.
How does it affect pregnancy?
PCOS can lead to complications during pregnancy such as gestational diabetes, pre-eclampsia, and premature birth. It’s crucial for pregnant women with PCOS to receive proper prenatal care to manage these risks.
Can men have a form of PCOS?
Men cannot have PCOS as it is a condition related to the female reproductive system. However, there are other conditions with similar metabolic and hormonal imbalances that can affect men.
Is weight gain inevitable with PCOS?
While weight gain is a common symptom of PCOS, it is not inevitable. A balanced diet, regular exercise, and maintaining a healthy lifestyle can help manage weight and other symptoms of PCOS.
Does a polycystic ovary always mean I have?
Having polycystic ovaries does not necessarily mean you have PCOS. Many women with polycystic ovaries do not have PCOS, and conversely, some women with PCOS do not have polycystic ovaries.
Can diet improve symptoms?
Yes, a healthy, balanced diet can significantly improve PCOS symptoms, help manage weight, and reduce the risk of other associated conditions like diabetes and heart disease.
Final Words
Polycystic Ovary Syndrome (PCOS) is a complex, multifaceted condition affecting numerous women worldwide. While it poses several challenges, understanding its nature, symptoms, and management strategies can significantly improve the quality of life for those affected.
The journey with PCOS is individual and varied, but with the right knowledge, support, and care, it is possible to navigate the challenges and lead a healthy, fulfilling life.