I see you’re here looking for some answers, and I’m glad you found your way to this article. Pregnancy can be a time of pure joy and excitement, but it can also bring with it a rollercoaster of emotions, especially when you’re experiencing something unexpected, like vaginal bleeding in early pregnancy. Believe me, I’ve been in your shoes, and I know how scary and confusing it can be.
But don’t you worry! I’m here to walk you through this journey as a friend who’s been through it all and has come out on the other side with a wealth of knowledge and understanding. Together, we’ll delve into the topic of vaginal bleeding in early pregnancy and shed some light on the reasons behind it, when it’s normal, and when you should seek medical attention. My goal is to help ease your concerns and empower you with the information you need to navigate this remarkable journey with confidence.
So, grab a cup of tea, wrap yourself in your coziest blanket, and let’s explore this topic together, because you’re not alone in this, my friend. Let’s dive in!
Dear ladies, being pregnant is a blessing and an exciting journey

In general most pregnancy will be an uneventful journey.
However, up to 1 in 5 (20%) pregnant women experience some vaginal spotting or vaginal bleeding during the 1st trimester of pregnancy (also known as early pregnancy).
1st trimester vaginal bleeding is defined as per vaginal bleeding in the first 12 weeks of pregnancy.
In early pregnancy, you may experience some perfectly harmless light vaginal bleeding when the developing embryo implants itself in the wall of your womb (implantation bleeding). This often happens around the time when your 1st period after conception would have been due.
What You Need to Know
Vaginal bleeding during early pregnancy is not uncommon and can be quite unsettling. However, it’s important to understand that not all bleeding during early pregnancy indicates a problem. In some cases, bleeding may be due to implantation, which occurs when the developing embryo implants itself in the wall of the uterus. Implantation bleeding is typically light and occurs around the time when your first period after conception would have been due.
It’s crucial to recognize the various causes of vaginal bleeding in early pregnancy, which include miscarriage, ectopic pregnancy, local causes such as cervical polyps and cervical cancer, bleeding after sex, and unexplained bleeding in normal pregnancies.
Causes of vaginal bleeding in early pregnancy:
Miscarriage (Spontaneous abortion)

Miscarriage occurs when the pregnancy ends before the 24th week of pregnancy.
Miscarriages are relatively common and up to 1 in 5 pregnancies ends in a miscarriage during the 1st trimester.
Commonly this usually presents with vaginal bleeding and abdominal pain, except for missed miscarriages where the woman can have no symptoms.
Miscarriages can be further categorized as threatened, complete, incomplete or missed and also further classified as sporadic or recurrent (>3 miscarriages).
Threatened miscarriage:
Threatened miscarriages involve a viable foetus (one with a demonstrated heartbeat) but the mother experience vaginal bleeding +/- abdominal pain. About half of these cases may progress into actual miscarriages while the other half can continue on to a normal full term pregnancy.
Incomplete miscarriage:
This is when there are still retained products of conception during the ultrasound scan. The cervical os may be open with products of conception being passed out. The patient would have to undergo a surgical procedure to remove the rest of the products from the womb otherwise a serious infection can occur.
Complete miscarriage:
Patients may present with a history of bleeding, abdominal pain and passage of foetal products. By the time the miscarriage is complete, bleeding and pain usually have subsided. Observation of the aborted foetus with the complete placenta will aid in diagnosis but the woman should have an ultrasound scan done to ensure that the uterus is empty.
Missed miscarriage:
Patients may or may not experience any bleeding or abdominal pain. Usually a missed miscarriage is picked up during ultrasound scanning which identifies an absent foetal heartbeat, indicating foetal demise. This is usually one of the most distressing types of miscarriage as there are usually no warning signs.
Risk factors for miscarriages:

- Endocrine disorder
This includes medical conditions such as low progesterone levels, thyroid disease, and poorly controlled diabetes.
- Abnormality in the number of chromosomes of the foetus (genetic aneuploidy)
– number and configuration of chromosomes is incompatible with life.
- Infection (e.g.: Chlamydia, gonorrhoea, herpes, listeria, mycoplasma, syphilis, toxoplasmosis, and ureaplasma.)
- Maternal age: risk of miscarriage increases with age. The greatest increase occurs after 35 years of age.
Other less common risk factors include occupational chemical exposure or radiation exposure.
Ectopic pregnancy
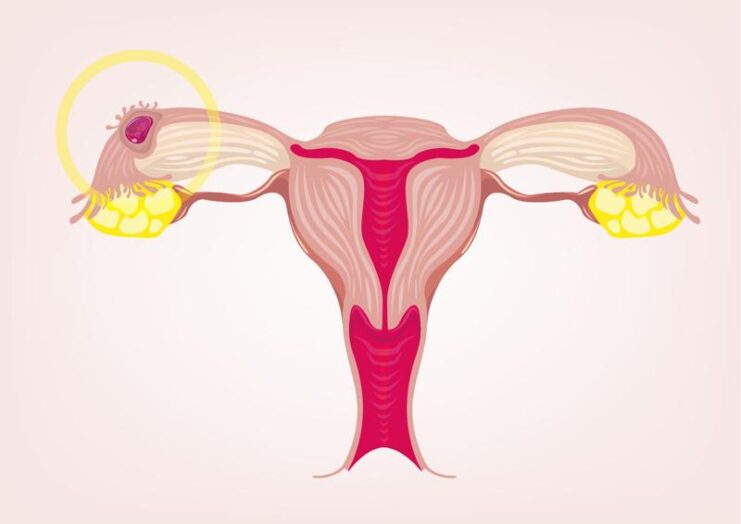
Ectopic pregnancy occurs when a fertilised egg implants outside the womb – for instance in the fallopian tube, ovary, etc. This can cause vaginal bleeding but more commonly associated with abdominal pain.
All pregnant women with vaginal bleeding +/- abdominal pain should have an ultrasound scan performed to identify the location of the pregnancy. Early diagnosis of ectopic pregnancy is key to preserving fertility, and preventing complications, which may lead to death.
Risk factors for ectopic pregnancy:
- Having a current intrauterine device (IUD)
- Previous history of ectopic pregnancy
- History of genital tract infection, including pelvic inflammatory disease, Chlamydia, gonorrhoea, etc
- Previous history of any fallopian tube surgery
- Current pregnancy conceived via In vitro fertilization (IVF)
- Smoking
Local causes – cervical polyps, cervical cancer
The majority of cervical polyps are non-cancerous and are not uncommon during pregnancy. Most of the time they do not cause any symptoms and you would not know they existed. Occasionally, these polyps can start to bleed on their own or through physical contact such as during sex.
Usually, polyps will get smaller and resolve after delivery and surgery is not needed during pregnancy unless there is constant bleeding or significant symptoms of discomfort.
Rarely, vaginal bleeding can be caused by changes in the cervical cells (pre-cancerous –> cancerous changes). If this is suspected during examination, a pap smear test may be performed. In most cases this should not affect your pregnancy and can be delayed until after the birth.
Bleeding after sex

During pregnancy, the cervix becomes softer and the blood supply to the area increases. As a result, sexual intercourse can sometimes cause light bleeding, which may last for a few hours to several days after sex.
This bleeding is generally harmless and does not pose a threat to the pregnancy. However, it is always essential to inform your healthcare provider if you experience any bleeding during pregnancy, as the bleeding may be unrelated to the changes in your cervix and could indicate an underlying issue that requires attention.
Unexplained bleeding (normal pregnancy)

In approximately 1/3 of pregnant women, the cause of vaginal bleeding is unknown. All investigations including ultrasound scans appear normal and the baby appears healthy and growing well. The bleeding may or may not happen again during the pregnancy but if you start to bleed again, it is advisable to see your doctor for an evaluation.
In summary, if you are pregnant and you are experiencing any vaginal bleeding +/- abdominal pain, I would strongly advise you to see a doctor for further evaluation.
Some preconception advice to help reduce the risk of miscarriage or ectopic pregnancy include:
- To have a pap smear test performed before getting pregnant as it would make it easier for the doctor attending you to know your updated pap smear status.
- Screen for any sexually transmitted infection (STI) especially if you are at risk of any before getting pregnant.
Seeking Medical Help: When to Consult Your Doctor
If you experience any vaginal bleeding during early pregnancy, it’s essential to consult your healthcare provider for a proper evaluation. They will be able to determine the cause of the bleeding and advise you on the appropriate course of action.
In some cases, your doctor may recommend additional testing, such as an ultrasound or blood tests, to ensure the health and well-being of both you and your baby.
Preconception Advice to Reduce Risks
To minimize the risks of complications during pregnancy, consider taking the following preconception measures:
- Schedule a preconception checkup: Consult your healthcare provider before trying to conceive. This appointment allows your doctor to assess your overall health, identify any potential risk factors, and offer recommendations for a healthy pregnancy.
- Update your Pap smear: Ensure you have an up-to-date Pap smear before getting pregnant. This will provide your healthcare provider with valuable information about the health of your cervix and help detect any precancerous changes.
- Screen for sexually transmitted infections (STIs): Get tested for STIs, especially if you are at risk. Untreated STIs can increase the risk of miscarriage and ectopic pregnancy.
- Maintain a healthy lifestyle: Adopt a balanced diet, exercise regularly, and maintain a healthy weight. This will help reduce the risk of pregnancy complications and improve your overall health.
- Avoid smoking and limit alcohol intake: Smoking and excessive alcohol consumption can increase the risk of miscarriage and ectopic pregnancy. Quit smoking and limit your alcohol intake to ensure a healthy pregnancy.
FAQ
Can sexual intercourse cause a miscarriage or harm my baby?
In a low-risk pregnancy, sexual intercourse is generally considered safe and does not pose a threat to the developing baby or increase the risk of miscarriage. However, if you have a history of complications or have been advised by your healthcare provider to avoid sexual activity, it is crucial to follow their recommendations.
How can I prevent bleeding after sex during pregnancy?
While it may not be possible to completely prevent bleeding after sex during pregnancy, you can take certain precautions to minimize the risk:
- Use gentle, slow movements during intercourse.
- Ensure adequate lubrication to minimize friction.
- Communicate with your partner about any discomfort you may be experiencing.
- Avoid deep penetration, which may cause irritation to the cervix.
- Consider trying alternative positions that are more comfortable for you.
Should I stop having sex if I experience bleeding after intercourse during pregnancy?
If you experience bleeding after sex, it is essential to consult your healthcare provider for an evaluation. They will be able to determine the cause of the bleeding and advise you on whether it is safe to continue engaging in sexual activity. In some cases, your doctor may recommend abstaining from sex for a period of time, especially if the bleeding is due to an underlying issue that requires treatment or monitoring.
Is it normal to experience pain during sex while pregnant?
Some women may experience discomfort or pain during sex while pregnant, as hormonal changes and the growing uterus can cause the pelvic area to become more sensitive. If you experience pain during sex, communicate with your partner and try different positions that may be more comfortable. If the pain persists or worsens, consult your healthcare provider for further evaluation.
Conclusion: Navigating Pregnancy with Confidence and Support
Experiencing vaginal bleeding during early pregnancy can be distressing, but it’s essential to remember that not all bleeding indicates a problem. Armed with knowledge and the support of your healthcare provider, you can navigate this incredible journey with confidence. Keep an open line of communication with your doctor and don’t hesitate to ask questions or express concerns. By staying informed and proactive, you can ensure the best possible outcome for both you and your baby.
Related Posts:
- The Causes of Vaginal Bleeding After Sex (Post…
- Foods To Avoid During Pregnancy: Nourishing Your Baby Bum
- 6 Signs You Need Help With DoorDash Fast Pay Not…
- Understanding Abnormal Vaginal Bleeding: Unraveling…
- Vaginal Infection: Symptoms, Causes, and Prevention
- Understanding the Signs of Pregnancy - Embarking on…












